First Aid for Children
Additional material to support your information poster, with a quiz to test your knowledge.


THE TECHNIQUES ON THIS WEB PAGE ARE NOT FOR use on INFANTS UNDER 1 YEAR-OLD
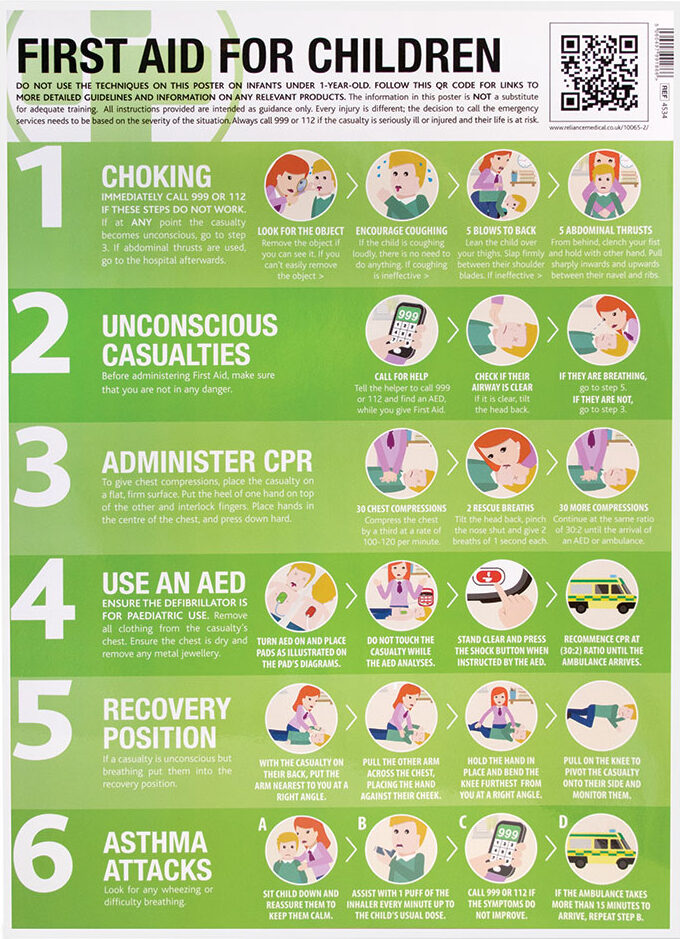
CHOKING
Prevention is better than cure! The best way to avoid choking is to make sure that small objects are kept out of your child’s reach.
However, if children under your care are choking on something, you need to take immediate action.

1. LOOK FOR THE OBJECT AND REMOVE IT IF POSSIBLE
If you can see the object, try to remove it. Don’t poke blindly or repeatedly with your fingers; as you could make things worse by pushing the object further in and making it harder to remove.

2. ENCOURAGE COUGHING
If the child is coughing loudly, there’s no need to do anything. Encourage them to carry on coughing and don’t leave them. If the child’s coughing is not effective, (e.g. it’s silent, or they can’t breathe in properly), shout for help immediately. If the child is still conscious, but either they’re not coughing or, their coughing is not effective, use back blows.

3. GIVE 5 BACK BLOWS
Lay a small child face down on your lap as you would a baby. If this isn’t possible, support your child in a forward-leaning position and give five back blows from behind. If back blows don’t relieve the choking and the child is still conscious, give abdominal thrusts. This will create an artificial cough by increasing pressure in the chest and helping to dislodge the object.

4. GIVE 5 ABDOMINAL THRUSTS
Stand or kneel behind the child. Place your arms under the child’s arms and around their upper abdomen. Clench your fist and place it between the navel and ribs. Grasp this hand with your other hand and pull sharply inwards and upwards. Repeat up to five times. Make sure you don’t apply pressure to the lower ribcage, as this may cause damage.
If you have had to use Abdominal Thrusts, always seek medical help afterward, even if the object has come out. Part of the object might have been left behind, or the child might have been hurt by the procedure.
Call 999 or 112 if these steps do not work.
If at any point the casualty becomes unconscious, administer CPR immediately.
Information based on the NHS’ “How to help a choking child.”
CARDIAC ARREST
Cardiac Arrest occurs when the heart suddenly and unexpectedly stops beating normally. When this happens, blood stops flowing to the brain and other vital organs. Ventricular Fibrillation, the most common cause of Cardiac Arrest, happens when the electrical activity of the heart becomes so chaotic, that it stops pumping and quivers instead. Sudden Cardiac Arrest can happen at any time. Immediate defibrillation and effective CPR can quadruple someone’s chances of survival. Using an Automatic External Defibrillator (AED), is easier than many people think, and they can be used by anyone, even without training.

1. MAKE SURE THE AREA IS SAFE
Whenever you approach an incident, your first consideration should be to make sure that the environment is safe. Check for electricity, fire, fumes, traffic, etc. Do NOT move the casualty unless you need to.

2. CHECK FOR A RESPONSE
Check if the casualty is conscious or not by calling their name and shaking their shoulders gently. You should also shout for somebody to help you. If someone can help, they should call the Emergency Services and locate an AED while you prioritise checking the casualty’s ABC’s, (Airway, Breathing, and Circulation, [CPR]).

3. CALL 999 OR 112
If someone has responded and has arrived to help, ask them to call and speak to the Emergency Services, otherwise, call them yourself. If possible, stay with the victim while making the call. It is a good idea to activate the telephone’s speaker function; this will aid communication with the Ambulance Service while you begin CPR.

4. EXAMINE AIRWAY
Check inside the child’s mouth for any obvious obstructions. If the airway is clear, turn the victim onto their back if they are not already on it. With your fingertips under the point of the victim’s chin, gently tilt the head back and lift the chin to open the airway.

5. CHECK BREATHING
Look, listen, and feel for normal breathing for no more than 10 seconds. In the first few minutes after Cardiac Arrest, a victim may barely be breathing, or just taking infrequent, slow, and noisy gasps. Do not confuse this with normal breathing. If you have any doubt whether breathing is normal, act as though it were not and start CPR without delay.



6. ADMINISTER CPR
GIVE 30 COMPRESSIONS
Kneel by the side of the victim and place the heel of one hand in the centre of the victim’s chest, (this is the lower half of the victim’s breastbone/sternum). Place the heel of your other hand on top of the first hand, then interlock the fingers of your hands and ensure that pressure is not applied over the victim’s ribs. Keep your arms straight. Do not apply any pressure over the upper abdomen or the bottom end of the bony sternum (breastbone). Position your shoulders vertically above the victim’s chest and press down on the sternum to a depth of 5–6 cm (approximately a third of the depth). After each compression, release all the pressure on the chest without losing contact between your hands and the sternum. Repeat 30 times at a rate of 100–120 compressions per minute.
GIVE 2 RESCUE BREATHS
After 30 compressions, open the airway again by using the head tilt and chin lift manoeuvre (as above), then give 2 rescue breaths. To give rescue breaths, use the index finger and thumb of the hand you have placed on the victim’s forehead, to pinch the soft part of the nose closed. Allow the mouth to open, but maintain the chin lift. Take a normal breath and place your lips around their mouth, making sure that you create a good seal. Blow steadily into the mouth while watching for the chest to rise, taking about 1 second as in normal breathing; this is an effective rescue breath.
Maintaining the head tilt and chin lift, take your mouth away from the victim and watch for the chest to fall as air comes out, then take another normal breath and blow into the victim’s mouth once more to achieve a total of two effective rescue breaths. Do not interrupt compressions by more than 10 seconds when delivering the two breaths, then return your hands without delay to the correct position on the sternum and give a further 30 chest compressions.
GIVE 30 MORE COMPRESSIONS
Continue with chest compressions and rescue breaths at a ratio of 30:2. If you are untrained, or unable to do rescue breaths, give chest compression CPR only, (i.e. continuous compressions at a rate of at least 100–120 per minute).

7. USE AN AED
Switch on the AED and attach the electrode pads to the victim’s bare chest by following the illustrations on the pad’s diagrams. You should ensure that the casualty is dry. Remove any metal jewellery or underwired bra’s as this can cause burns. If more than one rescuer is present, CPR should be continued while the electrode pads are being attached to the chest. Follow the spoken/visual directions of the AED. Ensure that nobody is touching the victim while the AED is analysing the rhythm.
If a shock is advised, deliver a shock.
Ensure that nobody is touching the victim, then push the shock button as directed. Immediately restart CPR at a ratio of 30:2. Continue as directed by the voice/visual prompts.
If no shock is indicated, continue CPR. Immediately resume CPR.

8. CONTINUE CPR
Do not interrupt resuscitation until a health professional arrives and tells you to stop, or you see the casualty definitely waking up, moving, opening their eyes, and breathing normally. It is rare for CPR alone to restart the heart. Unless you are certain the casualty has recovered, continue CPR. If your arms start to tire, see if another person can assist with the chest compressions.
For more information on the Resuscitation of Children, visit the Resuscitation Council’s: Paediatric Basic Life Support.
THE RECOVERY POSITION
If the casualty is unresponsive but is breathing normally, place them in the recovery position. N.B. Often, victims of Cardiac Arrest will have Agonal breathing. Agonal breaths are irregular, slow, and deep, frequently accompanied by a characteristic snoring sound. The presence of Agonal breathing is often interpreted incorrectly as evidence of a circulation and that CPR is not needed. This is incorrect. Bystanders should suspect Cardiac Arrest and start CPR if the victim is unresponsive and not breathing normally.
Putting an injured child in the recovery position will keep their airway clear and open. It also ensures that any vomit or fluid won’t cause them to choke.
If you are confident that the casualty is breathing normally, put them into the recovery position as follows:




N.B. If you suspect the casualty may have a spinal injury, DO NOT attempt to move them until the Emergency Services reach you.
SEVERE BLEEDING
If you are administering first aid to a casualty who is bleeding heavily, the main aim is to prevent further blood loss and minimise the effects of shock. In this case, shock does not mean emotional shock, but the life-threatening condition often caused by loss of blood.
Although First Aid must be given as soon as possible, you should always wear a pair of disposable gloves when you are dealing with a casualty that is bleeding, as it will protect both of you from the spread of any infections. Keep reassuring the child to keep them calm.
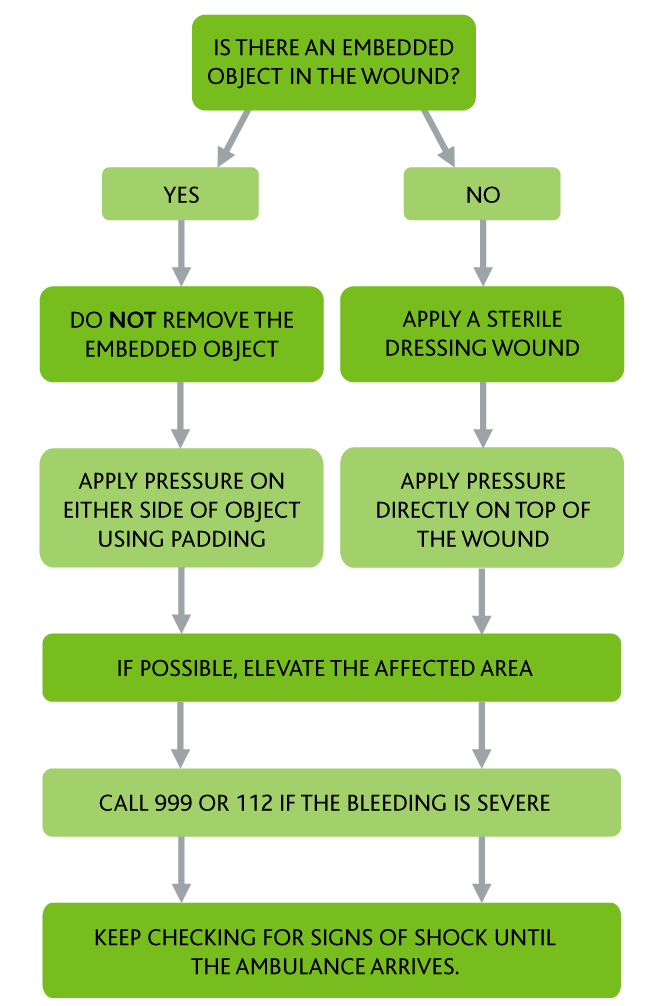
IF THERE IS NO OBJECT EMBEDDED INTO THE WOUND:
1. If possible, use a clean pad or dressing to apply pressure to the wound. Maintain the pressure until the bleeding stops.
2. If bleeding continues through the pad, apply another pad over the top and bandage it in place. Don’t remove the original pad or dressing, but continue to check that the bleeding has stopped.
3. If possible, elevate the injured area above the heart, while still applying pressure.
4. If the bleeding is severe, call 999 or 112 and ask for an ambulance as soon as possible.
5. Keep checking the casualty for signs of shock.
IF THERE IS AN OBJECT EMBEDDED INTO THE WOUND:
1. Do NOT remove any embedded objects; they can often be acting as a plug for the bleeding, and removing them will make it much worse.
2. Instead of applying pressure directly to the wound with a clean pad or dressing, apply pressure to either side of the embedded object instead.
3. If possible, elevate the injured area above the heart, while still applying pressure.
4. If the bleeding is severe, call 999 or 112 and ask for an ambulance as soon as possible.
5. Keep checking the casualty for signs of shock.
If a body part, (such as a finger), has been severed, place it in a plastic bag or wrap it in Clingfilm and make sure it goes with the casualty to hospital.
Information based on NHS’ First Aid: Bleeding.
ASTHMA ATTACKS
SYMPTOMS
Symptoms of an asthma attack to look out for:
• The child’s symptoms are getting worse, e.g. coughing, breathlessness, wheezing, or a tight chest.
• The child’s reliever/inhaler (usually blue coloured), is not relieving the symptoms.
• The child is too breathless to speak.
• The child’s breathing is getting faster and they can’t catch their breath.
• A child may also complain of a tummy ache.
The symptoms won’t necessarily occur suddenly. In fact, they often come on slowly over a few hours or days.


HOW TO TREAT AN ASTHMA ATTACK
If you think a child is having an asthma attack you should:
1. Remain calm, sit the child down, and tell them to take slow, steady breaths. Reassure the child and help them to remain calm; panicking will make things worse.
2. Fetch the child their inhaler and assist them with taking one puff on their reliever/inhaler (usually blue in colour), every minute, up to a maximum of 10 puffs.
3. If the child does not have their inhaler, or the symptoms are not being relieved by using the inhaler, call 999 or 112.
4. Keep the child as calm as possible until the ambulance arrives. If the ambulance takes more than 15 minutes to arrive, repeat step 2.
If the symptoms improve and you don’t need to call 999, tell the parent or guardian to make an appointment to see their GP or Asthma Nurse within 24 hours.
Information based on NHS’ Asthma attacks: what to do.
First Aid For Children Quiz
A short quiz to test your knowledge of first aid for children.

All information is for guidance only and correct at time of publication.



